Using AI to Automate Clinical Documentation in Hospitals
There is evidence that the food industry designs ultra-processed foods to be highly rewarding, to maximize craveability and to make us want more and more and more

Clinical documentation drains time from physicians and nurses—time that should be spent on patient care. AI-driven clinical documentation tools are stepping in to eliminate hours of manual typing and note entry.
Hospitals struggle with inaccurate, incomplete, or delayed documentation. These gaps reduce care quality, increase legal exposure, and create billing inefficiencies. AI helps by converting conversations, diagnoses, and observations into structured medical notes in real time.
AI-powered ambient scribe systems use natural language processing to listen during patient encounters and automatically generate EHR-ready notes. The system identifies medical terms, ICD codes, symptoms, and clinical actions with high precision, reducing manual corrections.
In practical use, emergency departments rely on AI scribes to accelerate triage, while outpatient clinics use them to streamline routine consultations. Specialists benefit even more—orthopedics, cardiology, and oncology have some of the heaviest note-taking burdens.
Time savings are measurable. Some hospitals report 40–60% reduction in documentation time per physician. Burnout decreases, appointment capacity increases, and coding accuracy improves.
As models evolve, AI will begin suggesting orders, highlighting missing clinical information, and predicting documentation gaps before audits occur.
AI documentation is shifting healthcare from “typing to care.” Hospitals that adopt early gain efficiency and higher clinical throughput.
More News
How AI Is Transforming Radiology Workflows: From Faster Scans to Accurate Diagnoses
There is evidence that the food industry designs ultra-processed foods to be...
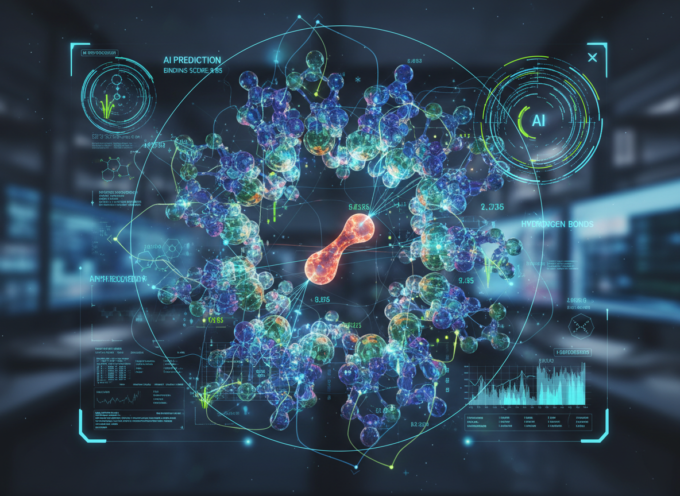
ByElizabethJune 5, 2024AI-Enhanced Drug Discovery: Cutting Development Timelines in Half
There is evidence that the food industry designs ultra-processed foods to be...
Byit.consultantMay 26, 2024How AI Predictive Models Are Improving Hospital Readmission Prevention
There is evidence that the food industry designs ultra-processed foods to be...
Byit.consultantMay 26, 2024











Leave a comment